What if You Could Choose Your Baby?
Icon of embryo in doctor’s hands (Natali_Mis, iStockphoto)
Icon of embryo in doctor’s hands (Natali_Mis, iStockphoto)
How does this align with my curriculum?
| Grade | Course | Topic |
|---|
Many people have had children using assisted reproductive technologies. But some of these medical biotech techniques can raise some ethical issues.
Time is flying by. It feels like you’re speeding your way through high school. You’re slowly starting to think about what adulthood might feel like. You might have even pictured yourself five to ten years from now. What does your life look like? Do you see yourself having children of your own?
As you read this article, I’d like you to imagine that your answer is yes. Now, how do those imaginary future children of yours come into the world?
Many people are conceived when a sperm fertilizes an egg inside a woman’s body, either through sexual intercourse or through artificial insemination. However, not all people can conceive children this way. About one in eight heterosexual couples will experience infertility. (1) Doctors diagnose infertility when a couple cannot conceive a child after a year of actively trying. These couples may choose to adopt a child. They might also decide to use assisted reproductive technologies (ART). This term refers to all treatments that involve manipulating eggs or embryos outside the human body in order to create a baby.
Did you know?
A wide range of people may choose to use ART, including couples (both heterosexual and homosexual) and single people wanting to have children.
Many people have had children through ART. But this technology can come with some ethical issues. Let’s look at what could happen when you combine an ART called in vitro fertilization with a screening technique called pre-implantation genetic diagnosis.
What is in vitro fertilization?
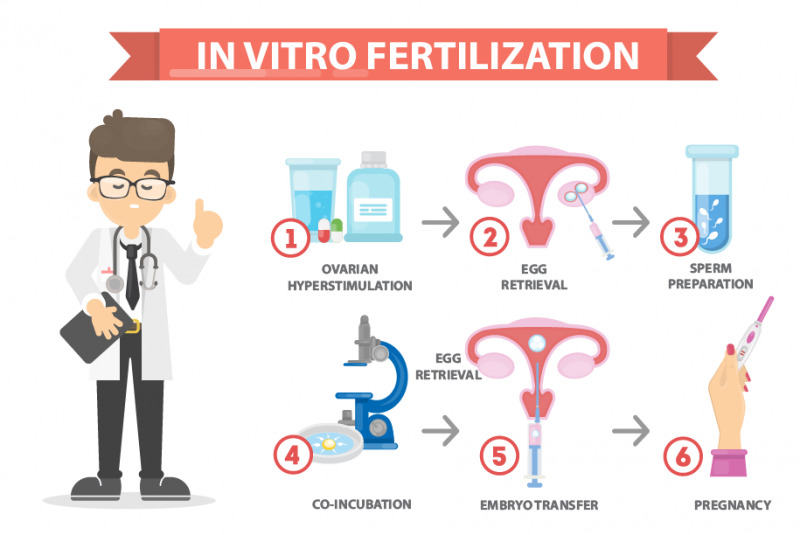
There are many different ART treatments. A popular one is in vitro fertilization (IVF). The main idea is to extract follicles (eggs) from a woman’s ovaries, fertilize them with sperm in a dish and then insert the fertilized egg into a woman’s uterus. Here are the specific steps:
- The woman trying to get pregnant takes hormone medication that alters her menstrual cycle. Instead of releasing one egg in a 28-day cycle, she releases several. This is called ovarian hyperstimulation (or superovulation). An embryologist measures the woman’s hormone levels to determine when her levels are right for to get pregnant.
- Once the woman is ovulating, an embryologist uses a needle and probe to retrieve eggs from her body. This can be uncomfortable, so the woman gets a local anesthetic (pain reliever) and sedation (medication to relax).
- The sperm is prepared.
- The woman’s eggs are fertilized with the sperm that same day. This step is called co-incubation (incubated together).
- The embryo (fertilized egg) is transferred (reinserted) into the woman’s uterus.
What is preimplantation genetic screening? What is preimplantation genetic diagnosis?
There are two other steps that parents-to-be can take just before the embryos are re-inserted. They can use techniques called pre-implantation genetic screening (PGS) and pre-implantation genetic diagnosis (PGD) to select specific embryos.
In PGS and PGD, embryologists remove a cell in a 5-day embryo. In PGS, embryologists screen the chromosomes of the embryo’s cells. They look for conditions such as Trisomy 21, which causes Down’s Syndrome.
In PGD, embryologists screen the genetic material of the cell. They look for gene mutations that cause genetic disorders, like cystic fibrosis. This may take up to several weeks. (2) Embryos that turn out to have problematic DNA are destroyed. The others weeks. (2) Embryos that turn out to have problematic DNA are destroyed. The others are kept for future IVF cycles.
Did you know?
PGD can test for more than 100 genetic disorders.
So what are the issues?
First, IVF and PGD are expensive techniques that many people can't afford. This could create a class divide between people who can afford to eliminate genetic diseases, and people who can’t.
Second, trying to eliminate disabilities with PGD may send a hurtful message to people who already live with disabilities.
Third, there are ethical questions. Critics worry that PGD may be associated with eugenic practices, or creating babies with “ideal” traits. Others critique the ethics in using the technique to create a saviour sibling. This is when a child is born to cure a sibling affected by a disease by donating their umbilical cord stem cells or tissues to their older sibling.
Finally, PGD could open the doors for sex selection. For example, in a technique called flow cytometry, scientists can use fluorescent dye to control an embryo’s sex. The X chromosome (female) will appear brighter than the Y chromosome (male) in a man’s sperm. Parents (with the help of scientists) could then choose what the sex of their baby would be. This technique, however, is not 100% effective.
Where does PDG stand today?
Different countries have adopted different regulations about PGD. In Canada, the Assisted Human Reproduction Act (AHRA) legislates ART. PGD is allowed for medical reasons, but it is unregulated. Sex selection is not allowed unless it is to prevent a sex-linked disorder -- a disorder that tends to be passed down via the X or the Y chromosome. An example is hemophilia, a disorder passed down via the X chromosome. People with hemophilia can bleed excessively because their blood does not clot properly.
Summing up...
A child can bring joy and happiness. But when that child comes into the world using complicated techniques, those techniques can raise ethical questions. IVF and PGD have helped many people dodge genetic conditions that run in families. But how far will this go?
What about you? If you could choose your baby, would you?
Did you know?
In Canada, donating sperm, eggs or embryos is legal. But buying, selling or exchanging them is not.
Starting Points
- Would you want to know the sex of your baby before it was born? Why or why not? Are there traits that you would be interested in knowing about? What traits in particular?
- Have you heard the term “test tube baby” before? What do you think it means?
- If you were to find out you could not get pregnant naturally, would you consider IVF? What other options would you consider, and why?
- Are procedures like IVF and PGD available to everyone? What barriers exist to the accessibility of IVF and PGD?
- What is the approximate cost to have one cycle of IVF done in Canada? Do provincial governments provide financial support to make IVF available to all people in Canadian society?
- Do you think that allowing people to use PGD for sex selection could have an effect on the demographics of a country? Why or why not?
- What does assisted reproductive technologies mean?
- What is infertility? When is a couple eligible for an IVF procedure?
- What is a sex-linked disorder? What is one exception to the sex selection restrictions in the Assisted Human Reproduction Act (AHRA)?
- How is assisted reproductive technology regulated in Canada? Why is regulation important?
- What media stories and/or reality television programming have you seen that has a connection to results of IVF procedures? Do you think these stories and programming helps promote IVF or does deter people from undergoing IVF procedures? Why or why not?
- This article and embedded video can be used in Health & Human Body and Engineering & Technology for teaching and learning related to reproductive technologies, medical biotechnology and medical ethics. Concepts introduced include infertility, artificial insemination, assisted reproductive technologies (ART), in vitro fertilization (IVF), follicles, ovaries, sperm, uterus, preimplantation genetic diagnosis (PGD), embryologist, X and Y chromosome, Assisted Human Reproduction Act (AHRA), sex-linked disorder and hemophilia.
- After reading the article and viewing the video, teachers could have students complete a Concept Definition Web for one of the key terms introduced, such as in-vitro fertilization (IVF) or pre-implantation genetic diagnosis (PGD). Ready-to use Concept Definition Web reproducibles are available in [Google doc] and [PDF] formats.
- After reading and viewing, teachers could also have students consider the issues associated with preimplantation genetic diagnosis from different perspectives (e.g., parents, siblings, family doctor, fertility specialist, priest or minister, journalist, etc.) using an Issues & Stakeholders learning strategy. Ready-to-use Issues & Stakeholders reproducibles are available in [Google doc] and [PDF] formats.
Connecting and Relating
- Would you want to know the sex of your baby before it was born? Why or why not? Are there traits that you would be interested in knowing about? What traits in particular?
- Have you heard the term “test tube baby” before? What do you think it means?
- If you were to find out you could not get pregnant naturally, would you consider IVF? What other options would you consider, and why?
Relating Science and Technology to Society and the Environment
- Are procedures like IVF and PGD available to everyone? What barriers exist to the accessibility of IVF and PGD?
- What is the approximate cost to have one cycle of IVF done in Canada? Do provincial governments provide financial support to make IVF available to all people in Canadian society?
- Do you think that allowing people to use PGD for sex selection could have an effect on the demographics of a country? Why or why not?
Exploring Concepts
- What does assisted reproductive technologies mean?
- What is infertility? When is a couple eligible for an IVF procedure?
- What is a sex-linked disorder? What is one exception to the sex selection restrictions in the Assisted Human Reproduction Act (AHRA)?
Nature of Science/Nature of Technology
- How is assisted reproductive technology regulated in Canada? Why is regulation important?
Media Literacy
- What media stories and/or reality television programming have you seen that has a connection to results of IVF procedures? Do you think these stories and programming helps promote IVF or does deter people from undergoing IVF procedures? Why or why not?
Teaching Suggestions
- This article and embedded video can be used in Health & Human Body and Engineering & Technology for teaching and learning related to reproductive technologies, medical biotechnology and medical ethics. Concepts introduced include infertility, artificial insemination, assisted reproductive technologies (ART), in vitro fertilization (IVF), follicles, ovaries, sperm, uterus, preimplantation genetic diagnosis (PGD), embryologist, X and Y chromosome, Assisted Human Reproduction Act (AHRA), sex-linked disorder and hemophilia.
- After reading the article and viewing the video, teachers could have students complete a Concept Definition Web for one of the key terms introduced, such as in-vitro fertilization (IVF) or pre-implantation genetic diagnosis (PGD). Ready-to use Concept Definition Web reproducibles are available in [Google doc] and [PDF] formats.
- After reading and viewing, teachers could also have students consider the issues associated with preimplantation genetic diagnosis from different perspectives (e.g., parents, siblings, family doctor, fertility specialist, priest or minister, journalist, etc.) using an Issues & Stakeholders learning strategy. Ready-to-use Issues & Stakeholders reproducibles are available in [Google doc] and [PDF] formats.
Learn more
How in vitro fertilization (IVF) works (2015)
This TED-Ed video (6:42 min.), with animation, illustrates the processes of in vitro fertilization.
Breeding out disease with PGD Testing (2016)
This video (5:04 min.) from Genesis Genetics explains why people may choose to use PGD testing, how it works, and the various steps involved.
How are genetic diseases inherited? (2010)
Genetic Disease Foundation gives a brief overview of genetic diseases, and the different ways they can be inherited.
Pre-implantation Genetic Screening / Diagnosis
The first video (3:10 min.) on this webpage from the Fertility Institute of Hawaii provides a good explanation of the difference between PGS and PGD.
An Introduction To Preimplantation Genetic Diagnosis (PGD) (2013)
This video (8:14 min.) by PGD Basics includes a strong focus on the ethical issues related to PGD.
References
American Pregnancy. (2019). Preimplantation genetic diagnosis: Benefits & concerns.
Devlin, H., & Sanderson, M. (2017). Editing the embryo: removing harmful gene mutations - Science Weekly podcast. The Guardian.
Genetic Disease Foundation. (n.d.). Hope through knowledge.
Government of Canada. (2013). Fertility.
Reproductive Health CDC. (2017). What is assisted reproductive technology?
Resolve. (n.d.). Fast facts. RESOLVE: The National Infertility Association.
Soini, S., Ibarreta, D., Anastasiadou, V., Aymé, S., Braga, S., & Cornel, M. et al. (2006). The interface between assisted reproductive technologies and genetics: technical, social, ethical and legal issues. European Journal Of Human Genetics, 14, 588-645. DOI: 10.1038/sj.ejhg.5201598