Can Your Own Cells Cure Cancer?
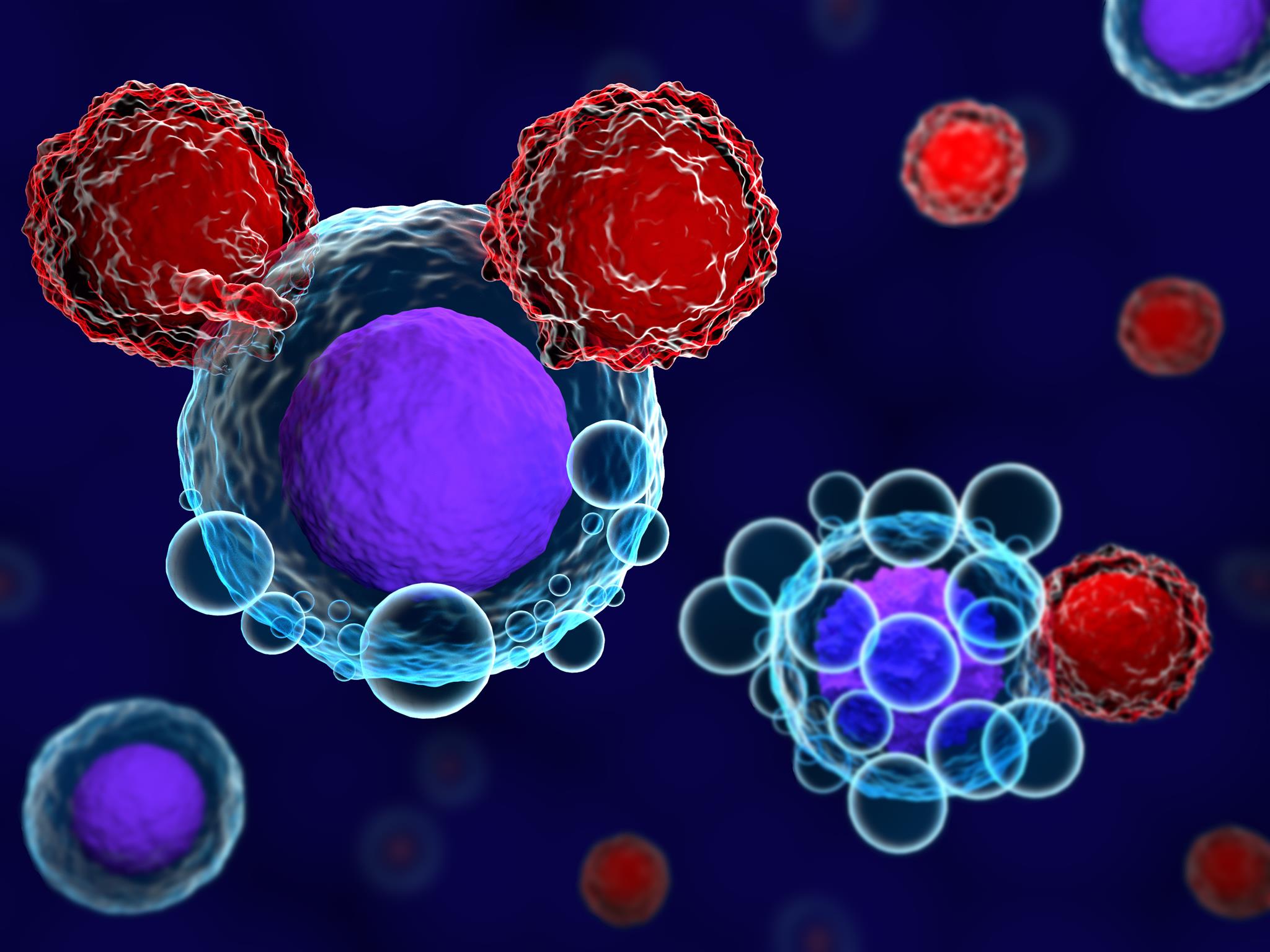
T cells and cancer cells - Image © Meletios Verras, iStockPhoto.com
T cells and cancer cells - Image © Meletios Verras, iStockPhoto.com
8.30
How does this align with my curriculum?
Curriculum Alignment
AB
10
Knowledge and Employability Science 10-4 (2006)
Unit C: Investigating Matter and Energy in Living Systems
NU
10
Knowledge and Employability Science 10-4 (2006)
Unit C: Investigating Matter and Energy in Living Systems
NT
10
Knowledge and Employability Science 10-4 (Alberta, 2006)
Unit C: Investigating Matter and Energy in Living Systems