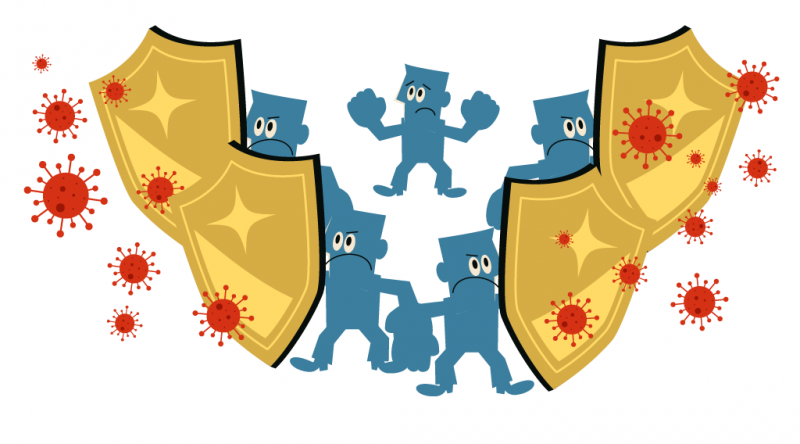
Herd Immunity: How Vaccines Protect the Most Vulnerable

Icon showing a syringe on a shield (johavel, iStockphoto)

Icon showing a syringe on a shield (johavel, iStockphoto)
8.04
How does this align with my curriculum?
BC
11
Science for Citizens 11 (June 2018)
Big Idea: Scientific processes and knowledge inform our decisions and impact our daily lives.
YT
11
Science for Citizens 11 (British Columbia, June 2018)
Big Idea: Scientific processes and knowledge inform our decisions and impact our daily lives.
BC
11
Life Sciences 11 (June 2018)
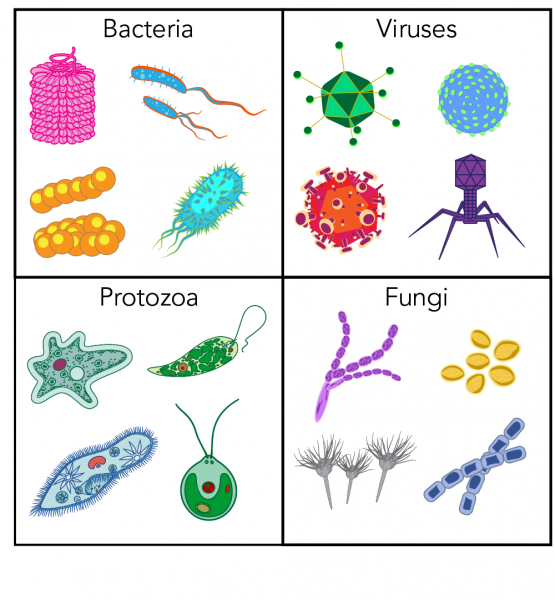
Big Idea: Life is a result of interactions at the molecular and cellular levels.
NU
11
Knowledge and Employability Science 20-4 (Alberta, 2006)
Unit C: Disease Defence and Human Health
YT
11
Life Sciences 11 (British Columbia, June 2018)
Big Idea: Life is a result of interactions at the molecular and cellular levels.
NT
11
Knowledge and Employability Science 20-4 (Alberta, 2006)
Unit C: Disease Defence and Human Health
NB
11
Sciences de la nature, 11e année (2005)
Thème 3: Microorganismes, système immunitaire et santé
YT
8
Science Grade 8 (British Columbia, June 2016)
Big Idea: Life processes are performed at the cellular level.
BC
12
Anatomy & Physiology 12 (June 2018)
Big Idea: Organ systems have complex interrelationships to maintain homeostasis